By Kate Hull // Photography by Shannon Corsi
—
The let-down reflex—a hormonal response created when a baby suckles at the breast—signals a mother’s body to release milk. For some, it can be a blissful sensation and moment of deep connection with their little one. I, however, have wondered many times since my son was born, Who in the world came up with that name? It sounds lovely when you read it, right? But when something isn’t going smoothly, the feeling of being let down by the process is a real kick in the postpartum pants.
I delivered my baby boy, Nathan, in August of 2021, and there are particular moments in the infancy of my motherhood journey I know I will never forget. The first is staring down at the blue-eyed, big-cheeked, chunky boy curled upon my chest only seconds after he came into the world. That feeling of overwhelming joy will be with me forever. The second happened a week later while sobbing into my own mother’s arms, upon realizing the heavy-duty, hospital-grade pump I had just driven from Jackson to my home in Victor, Idaho, on a Friday afternoon was missing a part. I was overwhelmed and filled with panic. Breastfeeding wasn’t working, and I didn’t understand it.
My milk seemed slow to come in. I felt like a failure, as my most important task—feeding my baby boy—was an unexpected uphill battle. I was blistered and bleeding (while still injured from delivery, with hormones lit up like a firework show) and left wondering, Why in the world are my breasts not doing their damn job?!


I pumped and pumped. My partner finger-fed our baby with a tiny tube. And, I used a nipple shield to help encourage a latch. I can barely remember when, but eventually things began to take shape. I found a pumping phalange that fit my breasts. (It’s not one size fits all, mamas!) I stocked up on healthy foods that encouraged an increased milk supply, and drank water like it was my job. I ate more lactation cookies than I ever thought possible. I even drank blue Gatorade because I heard it might help.
Did the old wives’ tales work?
I am not sure. What I do know, however, is that leaning on my partner and support from experts guided my uncertain ship forward.
If you are reading this—with a newborn in arms or during any chapter with your little one—I am not here to tell you there is a right or wrong way to feed your baby. What I do hope is that, by reading this, you’ll find resources, and maybe even solace, in a shared experience. Warts and all … blistered nipples and all … if I could go back to August 2021, here’s what I’d tell myself:

Be Flexible
Prior to Nathan’s birth, I, admittedly, hadn’t given much thought to breastfeeding. I knew I wanted to do it, but it wasn’t where my thoughts went as I dreamed and planned for the days to come. I wondered how I would transition into motherhood, who my baby boy would become, and how we’d make all the pieces fit. I assumed breastfeeding would just be another piece in the mamahood puzzle. When it wasn’t, I became relentless in my determination—at times, honestly, to the detriment of my mental health—and approached it with a ferocious commitment to make it be okay. Or at least my version of “okay.”
The lesson: Take a breath and let it be what it is.
“Breastfeeding is chosen for the health benefits to both mom and baby, and it is a valid and worthy goal to achieve,” says Kristie Karroum, an Idaho Falls-based international board-certified lactation consultant with Nurture Lactation Support, FNP-C, IBCLC, and Family Nurse Practitioner. “But it can also be challenging, and it’s a journey with changes.”
My secret to moving forward was, without question, a lactation consultation. Here in the Tetons, we are fortunate to have access to lactation support at regional hospitals like Jackson’s St. John’s Health and Eastern Idaho Regional Medical Center (EIRMC) in Idaho Falls. We also have private lactation consultants like Karroum who, thanks to the normalized world of Zoom calls, can offer telehealth-style consultations or appointments. After delivering at St. John’s, I was elated to find out that lactation support is not only available as frequently as needed, but it’s also a free service.
“As moms we do hard things because we want the best for our babies,” Karroum says. “It’s important to expect some challenges and know it is possible to seek out support to optimize working through them, but challenges also offer opportunities to demonstrate flexibility and grow our relationship with our baby. Women can be both determined and flexible.”
Determined and flexible. Say it with me: Flexible.

Seek Help
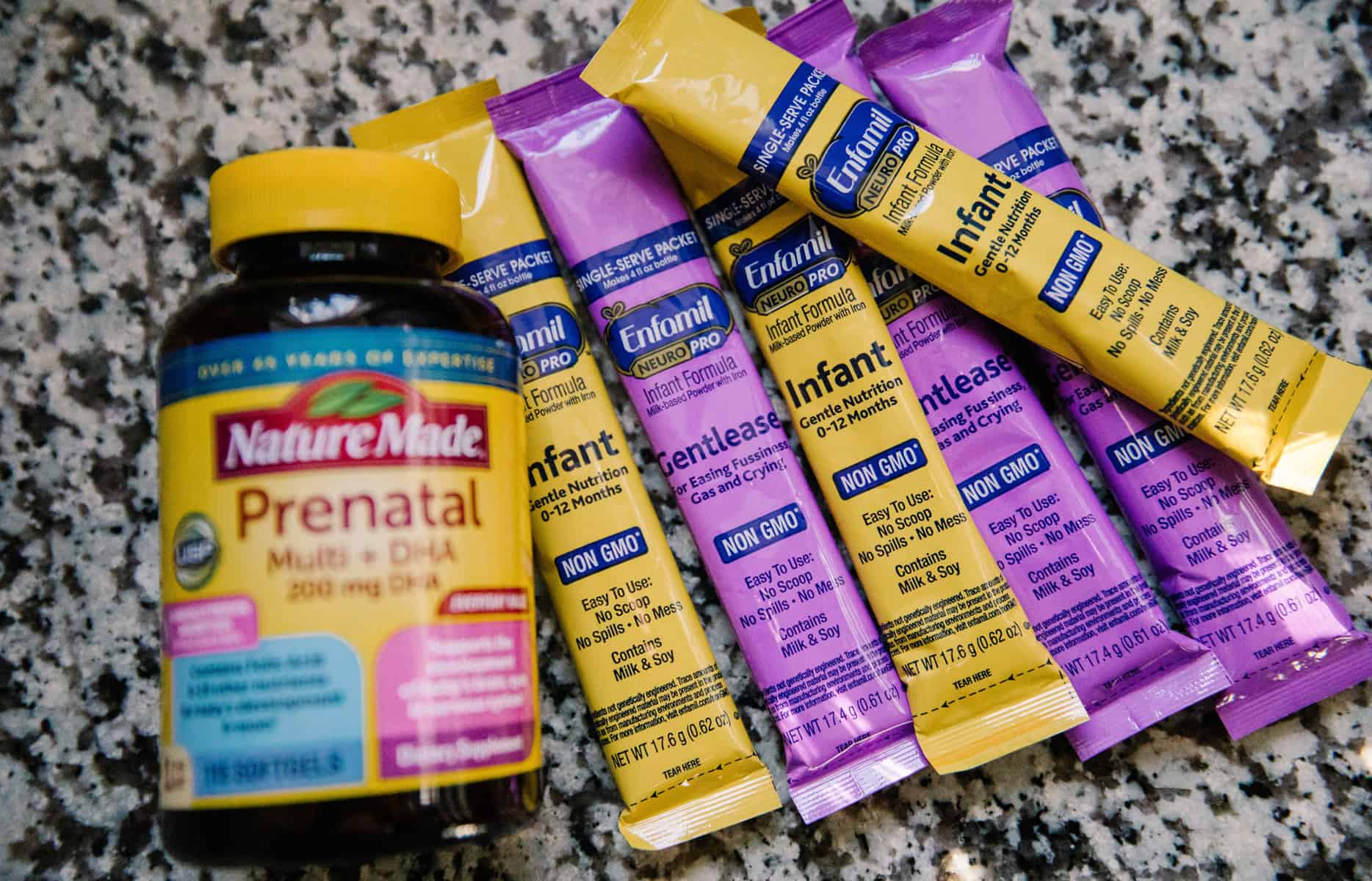
I became a frequent flyer at St. John’s. Janet Wood (RN, BSN, IBCLC, ANLC, OG), a certified lactation consultant, offered kindness and endless, knowledgeable support. Wood became the voice in my ear when I tried and tried again to get my baby to latch. “Fed is best,” she’d say. I worried that giving formula to my tiny guy was the wrong choice, while I painstakingly nursed my owned blistered nipples back to health. (I now know it wasn’t.) And, while my goal was to get my baby on the breast, I needed the grace and education Janet offered while I troubleshooted the problem.
Her go-to advice for new mamas: “I always say to keep the baby ‘in the kitchen’ in between the two ‘breastaurants,’” she says, with a chuckle. It may sound hokey, but she’s right. “Babies are hardwired to know how to find the breast and proximity matters. Skin-to-skin helps the neonate adjust to the extrauterine world.”
Wood is a pioneer in breastfeeding support for Jackson Hole. So much so, she is lovingly called “The Breast Whisperer” by many former clients, this one included. After a lengthy career as a labor and delivery nurse, she came to the Tetons in 1989 answering an ad for experienced labor and delivery nurses at St. John’s. “Over the years, I worked closely with Bonnie Pockat [RN, IBCLC at Teton County Public Health], and she encouraged me to become a lactation consultant for the hospital,” she says. “I focused on this specialty, and finally was able to create lactation support services in the spring of 2007 with my certification as an international board-certified lactation consultant.”
Now, Wood and her team offer lactation education and support during pregnancy, at the hospital during labor and delivery, and after the baby arrives. She also leads Teton Mammas, a group for new mothers who have questions, yet don’t need specific one-on-one consultation.
Wood’s approach is rooted in decades of knowledge, coupled with the understanding that every parent has a goal they are working to achieve. Her job is to help women reach it, even if the road takes a few unexpected turns.
“It bothers me that infant feeding is so black and white that we only ever pay attention to [either] breastfeeding or formula feeding,” she says. “Mixed-feeding came about to help babies gain weight while moms may be battling milk-supply issues. Any breastmilk feeding is beneficial to the baby and mother. The research tells us that even 50 milliliters of breastmilk per day is enough to have a positive impact. A single teaspoon of breastmilk contains over three million germ-killing cells.”
Trust Your Body
Wood also helped me better understand what my body needed. I drank water, took vitamins, worked to calm my mind, and asked for help when I needed it. I stopped comparing myself to other moms and took a break from scrolling Instagram.
Karroum offered similar support. She reminded me that every baby is different. At the time, I was sure my milk supply was low. Karroum helped me realize that I needed to trust my body. The problem was the solution: Nathan just needed to be on the breast as often as he could, with pumping in between. Slowly but surely, my body caught up.
“It is important to understand that it is okay to combine the information you are getting and find what works best,” says Karroum. “Every mother is going to have something that is a different fit. … You may have to go through a re-evaluation process. For example, ‘I wanted to exclusively breastfeed, but I am going to need to pump, or I am going to have [to supplement].’”
In both Wood and Karroum’s practices, the most common problems that women face are sore nipples and breasts, latch difficulty, and confusion surrounding milk supply. “There are some common myths about breastfeeding that can contribute to difficulty,” Karroum says. “One confusion,” she explains, “is thinking breastfeeding, as a natural act, is synonymous with ‘easy.’ Problems may arise, but they are solvable and flexible. Whatever the case, once we strip away the notion that it should be easy, we can better support moms on this journey.”


Advocate for Yourself
When breastfeeding enters the public sphere, it gets more complicated. How to do it, where to do it, and who gets to do it is the giant elephant in the nursery. The American Academy of Family Medicine reported that, for mother’s employed outside of the home, 67 percent began breastfeeding, but only 22 percent were able to continue breastfeeding by six months of age. That number drops to 10 percent at one year.
While it is federal law that employers must provide break time and a place for mothers to express milk during the day, many women report feeling unsupported despite this—leading to some ending their breastfeeding journey earlier than they would have liked. And laws for a woman’s right to nurse in public are left to the states. Idaho became the very last state to create such a law in 2018. Modern breastfeeding support is still in its infancy.
“We really need to reach employers and ensure they are allowing women the time and space to pump,” Karroum says. “Pumping is hard. It requires all this mental work to plan, make sure you have enough time, and think about the volumes. It is really challenging.”
It wasn’t until the mid-1950s that support groups for mothers even first cropped up. Nonprofit breastfeeding support group, La Leche League International, joined the conversation in 1956, led by seven women working to provide mother-to-mother support, encouragement, information, and education, among other things.
“As the years go by, I am often astounded by how we manage to add new wrinkles of complexity to something that should be easy, natural, and uncomplicated,” Wood says. “I can remember how unsupported/unpopular breastfeeding was back in the sixties and seventies. It wasn’t uncommon to hear from a mother, ‘I wanted to breastfeed, but the doctor told me that my baby was fussy due to my breastmilk and formula was better.’ Then, the rules devised to use formula feeding got applied to breastfeeding.”
Thankfully, thanks to advocacy and support, mothers are pushing the conversation forward and seeking out support.

What I’ve Learned
First, I am going to acknowledge my privilege. I had the ability to be home for four months thanks to a flexible job and support from my partner, family, and friends. I was given the space to decide what I wanted and to solve it without too many pressures from the outside world. I am more aware now than ever of that privilege. (There is a very important continual conversation to be had about the relationship between white privilege, classism, and breastfeeding rates, as well as support centering on the white experience.)
And, I wish I could say it all just came together overnight. Well, it didn’t.
I did, however, find a system that worked for both me and my little one. We got a groove going, and we smoothed out the wrinkles. The process—our process—became a wonderful, beautiful new version of what I expected. I learned that there is no one way to feed my baby, and whatever feels right to both of us is the right move.
So, to all you exclusively breastfeeding mamas: Go, you! To the formula-feeding mamas: Keep it up! To the combination feeding mamas: Heck, yes! No matter what you’re doing, you’re doing it. And when in doubt, find a good lactation consultant.

Breastfeeding Resources
—
In Wyoming
- St. John’s Health: stjohns.health/services/birth-center/lactation-support; 307-739-7572
- Teton Mammas: stjohns.health (Meets the second and fourth Wednesday of the month from 10 a.m. to 11 a.m.)
- Teton Postpartum: tetonpostpartum.com; tetonpostpartum@gmail.com; 303-601-3333
- Teton County Wyoming Health Department:tetoncountywy.gov/621/Best-Beginnings; 307-733-6401
- Teton TLC: Mark Tetenman, RN, CLC; tetontlc.com; 307-413-4977
In Idaho
- Eastern Idaho Public Health WIC: eiph.idaho.gov/WIC/Breastfeeding/wicbreastfeedingmain.html; 208-522-3823
- Eastern Idaho Regional Medical Center (EIRMC): prenatal breastfeeding class; eirmc.com; 208-529-7171
- La Leche Leauge of Idaho Falls: facebook.com/groups/lllif; 208-557-3922
- Madison Memorial Hospital: madisonmemorial.org/breastfeed-support; 208-359-6761
- Mountain View Hospital Lactation: mountainviewhospital.org/services/womens-center; 208-557-2729
- Nurture Lactation Support (Idaho Falls): Kristie Karroum, FNP-C, IBCLC; nurturemomandbaby.com; 208-569-9031 cell (text or call)
- Sonya Thompson, IBCLC (Rexburg): 208-351-0530




